The Procedure of Hysterectomy: An Expert Guide to Understanding This Pivotal Gynecological Surgery
The procedure of hysterectomy is a significant surgical intervention performed to address various benign and malignant gynecological conditions. As a common yet complex surgery, understanding every aspect of this procedure is crucial for women considering or advised to undergo it. This comprehensive guide aims to provide thorough insights into the procedure of hysterectomy, its types, indications, preparation, surgical methods, potential risks, recovery process, and long-term effects, thereby empowering women with knowledge to make informed health decisions.
Understanding the Procedure of Hysterectomy
A hysterectomy involves the surgical removal of the uterus. Depending on specific medical conditions and patient preferences, other reproductive organs such as the cervix, ovaries, and fallopian tubes may also be removed. The primary objective of this procedure is to eliminate symptoms stemming from, or risks associated with, various gynecological disorders.
Common Indications for Performing a Hysterectomy
The decision to perform a procedure of hysterectomy is based on careful evaluation by a qualified obstetrician and gynecologist. It is generally indicated in the following circumstances:
- Uterine fibroids causing significant symptoms like bleeding, pain, or pressure effects
- Endometriosis refractory to conservative treatments
- Chronic abnormal uterine bleeding that does not respond to medication
- Uterine prolapse where the uterus descends into or outside the vaginal canal
- Uterine or cervical cancer requiring surgical removal
- Adenomyosis with debilitating pain or heavy bleeding
- Pelvic pain of unknown origin that persists despite conservative treatments
Types of Hysterectomy: Tailoring Surgery to Patient Needs
The procedure of hysterectomy can be executed through various surgical approaches, classified primarily into four types according to the extent of removal:
1. Total Hysterectomy
Removes the entire uterus and cervix. It is the most common form of hysterectomy and is often chosen for benign conditions like fibroids or abnormal bleeding.
2. Subtotal (Partial) Hysterectomy
Involves removal of the uterine body while leaving the cervix intact. Suitable for women with benign conditions without cervical pathology.
3. Radical Hysterectomy
This extensive procedure includes the removal of the uterus, cervix, part of the vagina, and surrounding tissues. It’s typically performed in cases of gynecological cancers.
4. Hysterectomy with Oophorectomy and Salpingo-Oophorectomy
Sometimes, the removal of the ovaries and fallopian tubes along with the uterus is necessary, especially in cases requiring cancer treatment or certain genetic risk factors.
Surgical Methods of Performing the Procedure of Hysterectomy
The method chosen for the procedure of hysterectomy depends on the patient's condition, anatomy, and surgeon expertise. Major approaches include:
1. Abdominal Hysterectomy
Performed via an incision in the lower abdomen (laparotomy), this traditional approach provides direct access to the pelvic organs. It offers excellent visualization for large or complex cases but involves a longer recovery period.
2. Vaginal Hysterectomy
Involves removal of the uterus through the vaginal canal. It typically results in less pain, shorter hospital stay, and quicker recovery. Suitable for women with uterine prolapse or smaller uteri.
3. Laparoscopic Hysterectomy
A minimally invasive technique utilizing small abdominal incisions and a camera (laparoscopy). It provides excellent visualization, less postoperative discomfort, and faster return to daily activities.
4. Robotic-Assisted Hysterectomy
An advanced form of laparoscopic hysterectomy where robotic technology offers enhanced precision, flexibility, and control during surgery. It is especially advantageous for complex cases or larger uteri.
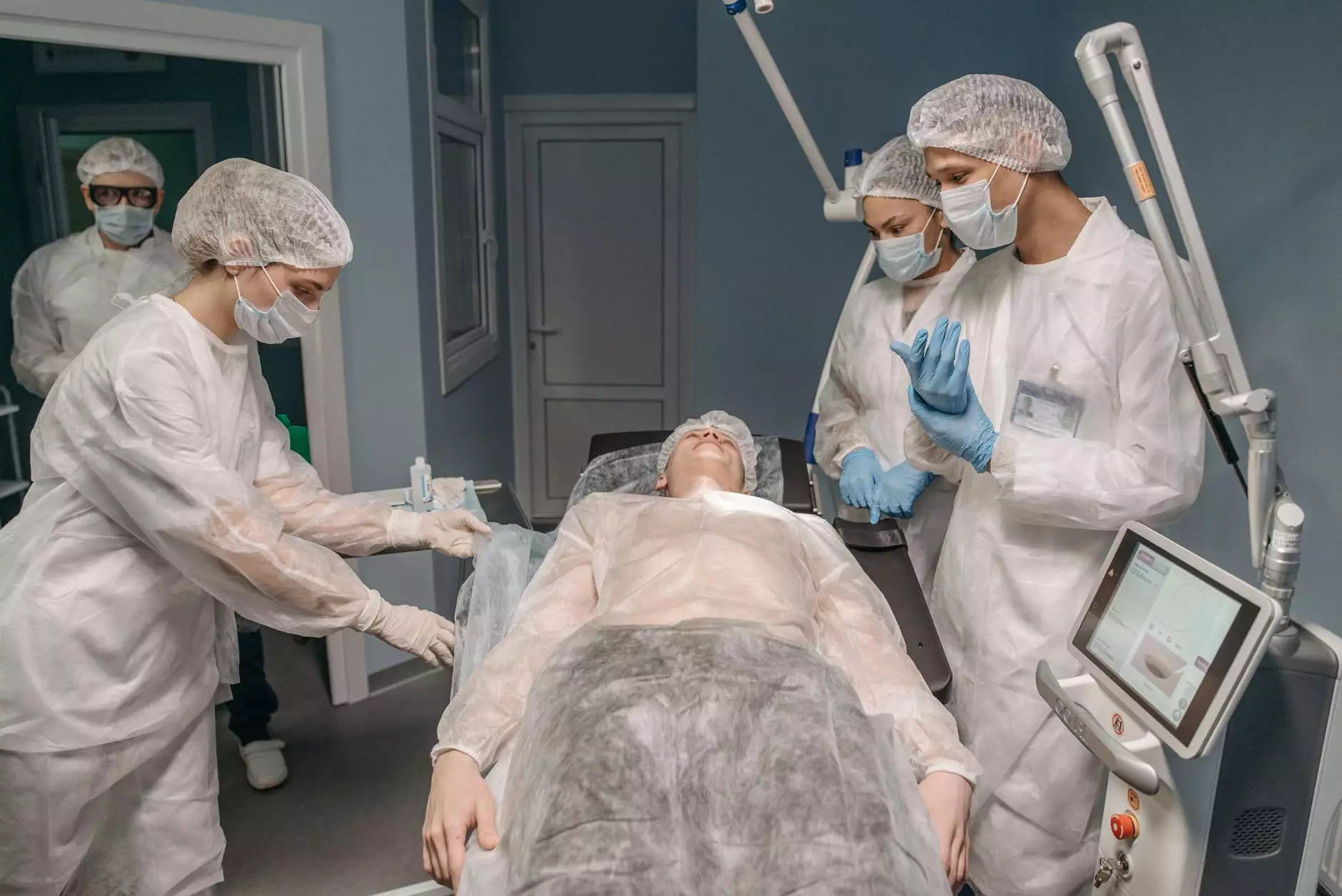
What to Expect During the Procedure of Hysterectomy
Before the surgery, patients undergo thorough medical evaluation, including physical exams, imaging tests, and blood work. The surgery is performed under general anesthesia, ensuring the patient is unconscious and pain-free during the procedure.
During surgery, the surgeon carefully isolates the uterus, controls blood vessels, and removes reproductive organs according to the chosen approach. Postoperative protocols focus on pain management, infection prevention, and early mobilization.
Potential Risks and Complications of the Hysterectomy Procedure
Although considered safe, like any surgery, the procedure of hysterectomy carries potential risks, including:
- Bleeding or excessive blood loss
- Infection at the surgical site or pelvis
- Injury to surrounding organs such as the bladder, intestines, or ureters
- Adverse reactions to anesthesia
- Blood clots in the legs or lungs
- Hormonal Changes especially if ovaries are removed, potentially leading to early menopause symptoms
- Pain or discomfort during recovery period
Postoperative Care and Recovery After the Hysterectomy
Postoperative recovery varies based on the surgical method, patient health, and the extent of surgery. Key aspects include:
- Hospital Stay: Typically ranges from 1 to 3 days for minimally invasive methods, longer for abdominal surgeries.
- Pain Management: Use of prescribed pain relievers to ensure comfort.
- Wound Care: Keeping incision sites clean and dry.
- Activity Restrictions: Avoid heavy lifting, strenuous activity, or sexual intercourse for several weeks.
- Follow-up Appointments: Regular visits to monitor healing and address any concerns.
Long-Term Effects and Considerations Following the Hysterectomy
The procedure of hysterectomy can significantly impact a woman's life, both physically and psychologically. Important considerations include:
- Menopause: If ovaries are removed, abrupt menopause may occur, necessitating hormone replacement therapy.
- Fertility: Complete removal of the uterus results in infertility. Women should discuss family planning options before surgery.
- Emotional and Psychological Impact: Some women experience grief, depression, or anxiety post-surgery, requiring counseling or support.
- Physical Changes: Possible changes in sexual function and pelvic support.
Choosing a Skilled Surgeon for Your Hysterectomy
Given the complexity and importance of the procedure of hysterectomy, selecting an experienced and reputable surgeon is paramount. Expertise ensures optimal surgical outcomes, minimized risks, and proper handling of any intraoperative challenges.
At drseckin.com, you can find leading obstetricians & gynecologists dedicated to providing personalized, high-quality care for women considering or undergoing a hysterectomy. Their extensive experience and commitment to excellence make them a trusted choice for your gynecological health needs.
Conclusion: Empowering Women Through Knowledge of the Procedure of Hysterectomy
Understanding the procedure of hysterectomy in detail demystifies this common surgical intervention and helps women make informed health decisions. Whether contemplating surgery for benign conditions or managing malignancies, knowing the types, methods, risks, and recovery expectations allows for proactive planning and peace of mind.
If you or someone you know is facing this decision, consult with qualified gynecologists at drseckin.com for personalized advice, comprehensive evaluations, and expert surgical care tailored to your individual needs.
Remember, your health journey is unique and important. Trust in professional expertise, stay informed, and prioritize your well-being at every step.









